
- What is Brachial Plexus
- How Brachial Plexus is diagnosed
- Types of Brachial Plexus Injuries
- Brachial Plexus Treatment
- Erb’s Palsy Injury
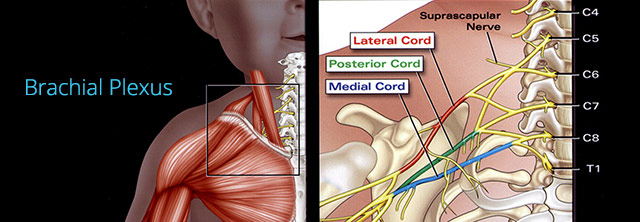
What is Brachial Plexus
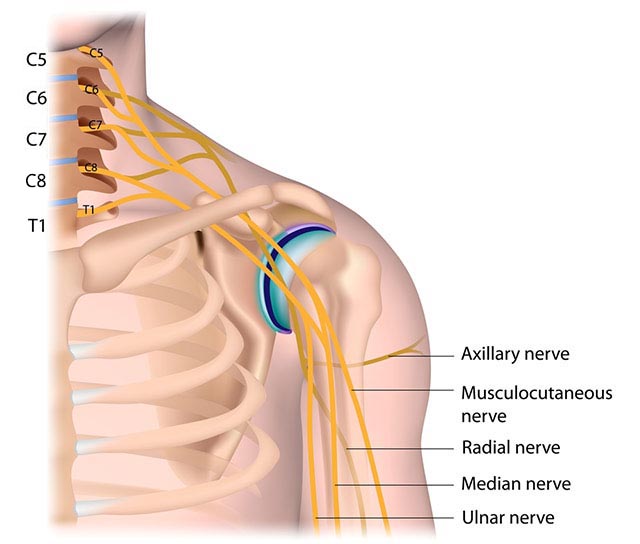
The brachial plexus is composed of several nerves from the cervical spine that coalesce at the base of the neck like a “fuse box”. They intermingle to form the nerves that innervate the entire arm and shoulder. During difficult birth deliveries, this plexus of nerves can be stretched and even ruptured, producing varying degrees of paralysis. This is the short answer to “What is Brachial Plexus?”. This injury still occurs in roughly two per thousand births.
In brief, nerves exit the spinal cord in the lower neck and travel to an area underneath the collar bone, where they coalesce to form the brachial plexus – almost like a fuse box. It is here that these nerve roots intermingle to emerge as the major nerves that innervate the shoulder, arm, and hand. Those nerve roots are the fifth, sixth, seventh, and eighth cervical nerve roots (cervical = in the neck) and the first thoracic nerve. Occasionally the fourth cervical or the second thoracic root is included.

How Brachial Plexus is diagnosed
When your new born baby is moving his or her arm, hand or fingers awkwardly, or lacks strength or reflexes, or you can visually detect deformation of your baby’s arm and/or hand, you ought to have your baby tested for Brachial Plexus injuries.
When an infant in the newborn nursery is noted to lack movement of the upper extremity, a physical exam determines the presence or absence of non-neurologic injuries. Birth trauma may fracture the clavicle, humerus, ribs, or even the femur. A limb fracture will behave as pseudoparalysis, that is, the baby won’t move the injured limb. A fracture alone may make the limb seem paralysed as the baby’s protective mechanism shuts down usage. Again, as in autos, a headlight broken does not exclude a wiring loss to that same headlight. Bulb replacement might not result in luminance. Brachial plexus injury may occur along with fracture. In the presence of a fracture the infant is protected (by, say, pinning the extremity to the torso by sling and swathe) for about 10 days. Though rare, acute shoulder or elbow dislocation can occur at birth. This needs to be recognized and treated as well.
When brachial plexus injury has occurred without an associated fracture or dislocation, traditionally, the affected arm has been, in a similar manner, pinned empirically (the idea being to protect the recently injured plexus). There is no data supporting that. We believe that immediate gentle restricted motion should be instituted, and no pinning or immobilization is routinely done. Stiffness is the problem. That’s what we seek to preempt.
There are several testing methods that may be conducted to diagnose Brachial Plaxus injuries. They include: Blood test, X-Rays, Ultrasound, MRI, EMG (Electromyogram) and Nerve Conduction Tests.
Brachial Plexus is not only caused by a child’s birth injury but is also a disease called Parsonage Turner syndrome. Young men (including teenagers) are at higher risk of getting this disease than any other age or gender.
In rare cases, a disorder called Brachial Neuitis was causing Brachial Plexus. Brachial Neuritis can be preceded by Varicella-Zoster Infection (cause of Chickenpox and Herpes.)
It is difficult to tell by today’s diagnostic tests what the exact nature and extent of the injury is and its potential to heal and recover. That is why initial management is a wait and see. But wait how long? And, see what? Unfortunately for prognostication (predicting what will be,) the degree and mix of injury, and the magnitude and rate of recovery vary from patient to patient. We, therefore, believe that each patient should have a unique treatment regiment prescribed. There are certain nuances to the natural history of this condition that if ignored, will have a significant impact on the final result.
Types of Brachial Plexus Injuries
Cause of Brachial Plexus Injuries
Brachial Plexus injuries occur during birth. The baby may become stuck when the head or the shoulder is unable to clear the mother’s pelvic outlet. In trying to get the baby delivered before any serious breathing or circulation problem occurs, traction on the head or shoulder may stretch nerve roots. Traction could even pull one or more roots out of the spinal cord.
Different Types of Brachial Plexus Injuries
Brachial Plexus injuries such as these occur roughly 2 times every 1000 births. They have traditionally been grouped into three categories:
Erb’s Palsy: A condition resulting from injury during birth which affects the C5, C6, and sometimes C7 nerve roots. This type is the most common type and fortunately has the best prognosis. The children affected have full use of the hand and fingers, but the function of the shoulder, elbow and forearm are affected. Read more>
Total Plexus Palsy: A condition which involves all roots of the brachial plexus. The entire upper extremity is affected, and this has the poorest prognosis of these injuries.
Klumpke’s Paralysis: A condition which occurs in well less than 1% of the cases involves just the lower roots (C8, T1). These children have normal use of the shoulder and elbow but weakness and/or paralysis in the fingers and the hand.
Even though we classify these injuries into these three broad categories, that is, into three generalities, the fact is that each patient’s injury is unique and typically much too complex to fit neatly into this classification system.

Brachial Plexus Treatment
Although physicians have treated this condition with a minimalist approach for more than 60 years, recent advances in microsurgical techniques and neurophysiologic monitoring now enable novel approaches to these severe injuries. Through research, remarkable progress has been made over the past 20 years. Nerve grafting, shoulder reconstruction, release of contractures, innovations in occupational therapy, splinting and casting are among the treatments that have become available.
In the natural history of brachial plexus birth injuries, according to some neurology texts, recovery of the injured plexus and nerves may occur over the first 6 years of life. During this time the child may completely recover or the clinical progress may plateau. Our goal is to maintain full motion of all joints, primarily through an ongoing intense therapy program. If recovery falters or plateaus, there are certain specific indications for interventions.
Erb’s Palsy Injury
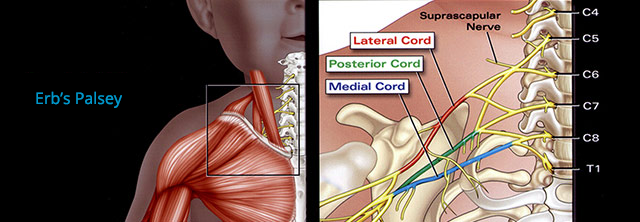
Difference between Erb's Palsy and Brachial Plexus
Erb’s Palsy is a condition resulting from injury during birth which affects the C5, C6, and sometimes C7 nerve roots. This type is the most common type and fortunately has the best prognosis. The children affected have full use of the hand and fingers, but the function of the shoulder, elbow and forearm are affected. When nerves in the upper part (nerve roots from C5 to C7) of the brachial plexus bundle are damaged, it is called Erb’s Palsy.
Erb's Palsy Conditions
Depending on the severity of the injury, Erb’s Palsy affects your child’s ability to move his/her arm(s), wrist(s) and hand(s) differently. If you see your child wiggling fingers but not moving his/her arm, hand or wrist, or even it looks paralyzed, you need to consult your physician. There are non-surgical interventions for most cases and surgical treatments for more severe cases.